The Significance of Medication Errors in Thailand
Patient safety is one of the most critical issues in Thailand’s healthcare system, with medication errors (ME) representing a significant problem that can potentially cause severe harm or even death. Thousands of medication errors are reported annually, but there remain limitations in analyzing this data effectively.
The Healthcare Accreditation Institute (HA) has initiated the National Reporting and Learning System (NRLS) to monitor and analyze adverse events, including medication errors. However, traditional analysis methods have inherent limitations since most data is recorded in free-text format, making systematic analysis challenging.
Types of Medication Errors in Thailand
Data from 2018-2024 reveals several significant types of medication errors:
- Wrong Medication – Examples include dispensing Etoxin instead of Tamiflu, or Cefotaxime instead of Ceftriaxone
- Wrong Route – Such as administering Haloperidol intravenously instead of subcutaneously
- Wrong Strength – For instance, dispensing Warfarin 5 mg instead of 2 mg
- Wrong Amount – Approximately 87,000 reported incidents
- Omitted Medication – Failure to administer prescribed medication
- Wrong Timing – Medication administered at incorrect times
- Unnecessary Medication – Administration of medication exceeding clinical necessity
Limitations of Traditional Reporting Systems and Opportunities for Development
Incident reports in NRLS predominantly contain valuable details in free-text format, including:
- Information comparing prescribed medications with those actually administered (names, dosages, routes)
- Incident locations and severity levels
There are important reasons for using free-text reporting:
- Medication incidents are complex and multifaceted, requiring highly detailed categories if dropdown systems were implemented
- Dropdown menus often overwhelm healthcare staff, exceeding their working memory capacity, resulting in incomplete or inaccurate data selection
 Applying AI and NLP in Medication Error Analysis
Applying AI and NLP in Medication Error Analysis
Artificial Intelligence (AI) technology can effectively address the limitations in analyzing free-text data, particularly through:
1. Named Entity Recognition (NER) Technology
NER systems can automatically identify critical medical details such as medication names, dosages, administration routes, and timing from report text.
2. Entity Linking
This connects information identified through NER with structured databases like SNOMED CT, enabling standardized analysis across medical institutions.
3. Transformer-based Models
These models excel at context analysis, increasing the accuracy of error classification by understanding nuances and contexts in NRLS reporting.
4. Classification Models
Classification models combining transformer-based models, rule-based algorithms, and Large Language Models (LLMs) can efficiently categorize medication errors.
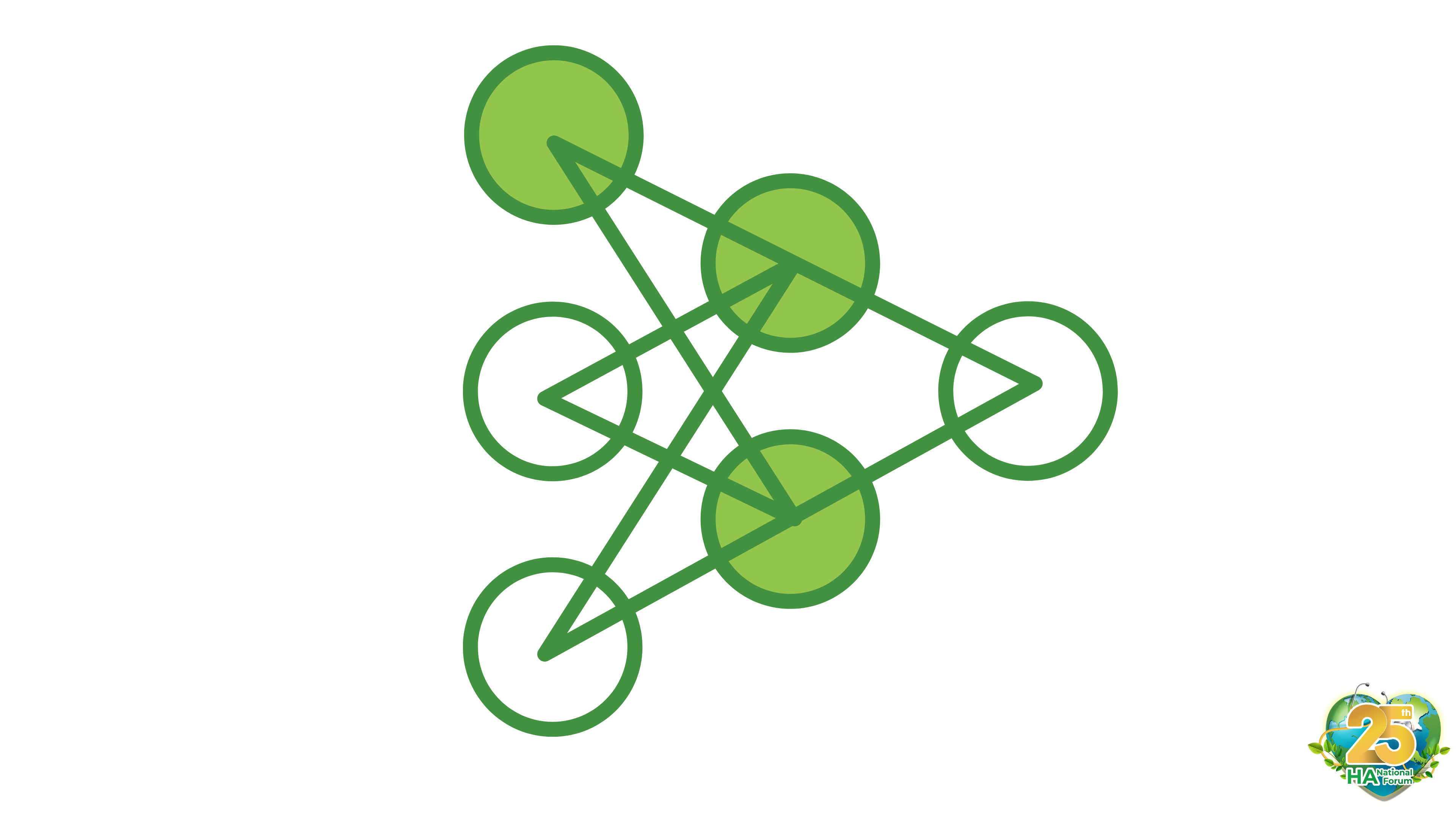
5. Visualization Tools
Tools like sunburst diagrams and bipartite graphs help visualize relationships between error types and differences between intended medications and those actually administered.
 Benefits of Using AI for Medication Error Analysis
Benefits of Using AI for Medication Error Analysis
Insights derived from AI-powered analysis can lead to evidence-based policy development, such as:
- Clear separation of medications with similar names or appearances
- Implementation of barcode medication administration systems
- Mandatory double-check procedures by healthcare professionals
Future Challenges
Despite AI implementation, a significant challenge remains in the underreporting of medication errors, limiting data analysis compared to systems in countries like the United States. Advancing AI analysis toward fully data-driven policymaking will help reduce medication errors and sustainably improve the efficiency of Thailand’s healthcare services.
Conclusion
Applying AI and NLP technologies to medication error analysis represents a crucial step in enhancing patient safety in Thailand. Healthcare professionals can leverage insights from AI analysis to improve practices and effectively reduce medication errors.
Bunnasorn Techajumlernsuk
Keywords: patient safety, medication errors, artificial intelligence, natural language processing, NLP, Thailand healthcare system, transformer-based technology, large language models